As a psychologist, I’ve met hundreds of people with bipolar disorder, and no two stories are the same.
One client couldn’t stop starting new businesses every few months, then vanishing from friends during “shutdown weeks.” Another felt like her brain was “plugged into lightning” one week and trapped in cement the next.
Neither of them knew they had bipolar disorder. They just thought something was wrong with them.
Bipolar disorder affects over 45 million people worldwide, yet many go undiagnosed for years, because their symptoms don’t look like the typical “mania and depression” we see in movies or Google results.
It’s not always extreme. Sometimes, it’s subtle. Quiet. Confusing. Dismissed.
In this article, I want to walk you through the less obvious signs of bipolar disorder, the ones that show up in thoughts, energy, sleep, and shame.
The ones that make people wonder, “Am I just being dramatic?” or “Why can’t I stay stable even when life is fine?”
Because the truth is, bipolar disorder doesn’t look the same for everyone.
And if you’ve ever felt caught between emotional extremes and can’t explain why, you’re not broken. You just might need the right lens.
What Is Bipolar Disorder (Really)?
Bipolar disorder is more than just feeling happy one day and sad the next. It’s a chronic mood disorder where your emotional states swing between two extremes mania (or hypomania) and depression.
But here’s the part most people don’t realize: these episodes don’t always look dramatic. In fact, some people live with it for years before they even realize something is wrong.
As a psychologist, I often meet clients who say things like:
“I thought I was just inconsistent.”
“I’m either too much or nothing at all.”
“Sometimes I don’t sleep for 3 nights straight… and then I crash.”
What they’re describing are signs of mood dysregulation that go deeper than stress or personality.
Bipolar disorder affects the way your brain regulates energy, emotions, motivation, sleep, and even decision-making.
The 3 Most Common Types of Bipolar Disorder:
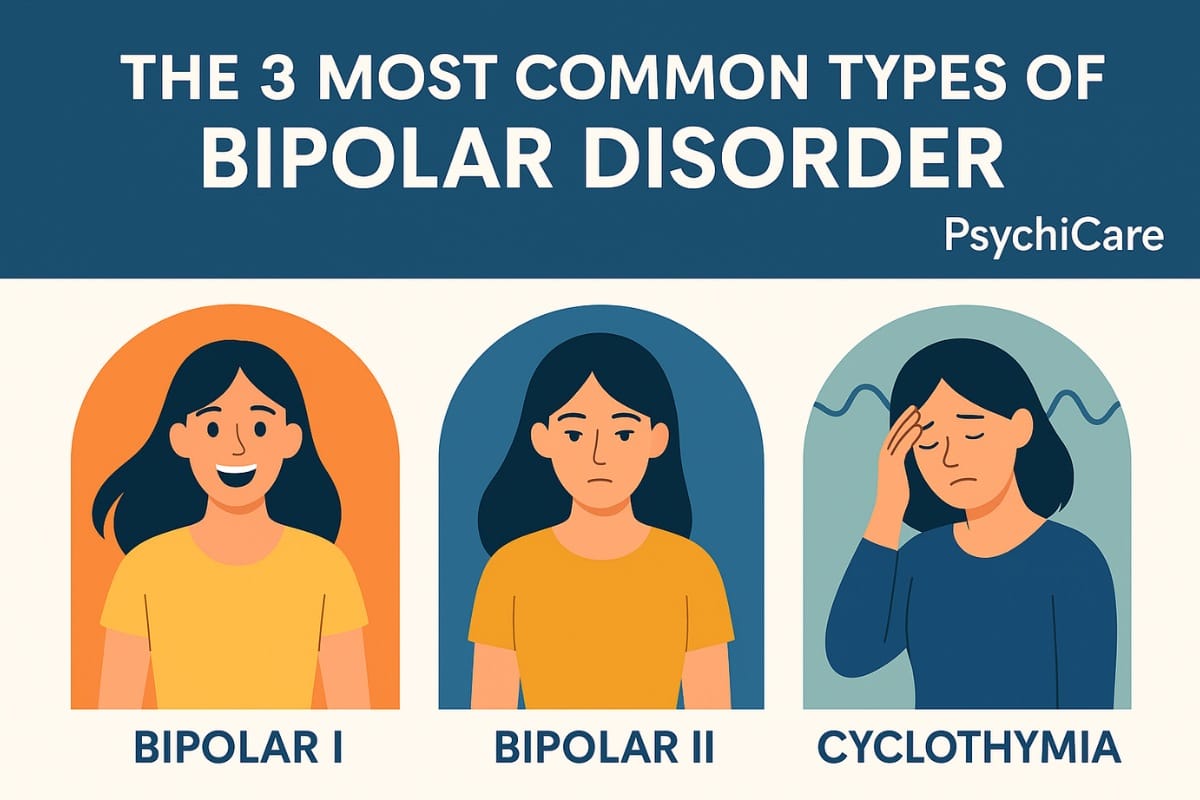
- Bipolar I Disorder
Full-blown manic episodes (often lasting a week or more) with or without depression. - Bipolar II Disorder
Patterns of hypomania (less intense than mania) and major depressive episodes. Often missed or misdiagnosed as just depression. - Cyclothymia (Cyclothymic Disorder)
Chronic, low-grade ups and downs that don’t meet full criteria for mania or major depression but still disrupt life.
Some people experience mixed episodes, where symptoms of both mania and depression appear together, like having racing thoughts and suicidal despair at the same time. These are often the most dangerous and misunderstood.
7 Lesser-Known Symptoms of Bipolar Disorder
Not all bipolar symptoms look like dramatic highs or deep lows. Some of the most disruptive, scary, and confusing signs are the ones people rarely talk about and often don’t connect to mental illness at all.
Here’s what I’ve seen again and again in therapy sessions and what people on Reddit, Quora, and YouTube are quietly asking about:
Dissociation and Emotional Detachment
People with bipolar disorder often describe feeling “outside their body” or emotionally numb, especially during rapid mood shifts or mixed episodes.
“It’s like I’m watching myself live, but I’m not there.”
This symptom is rarely discussed but incredibly common, especially during mixed affective states.
Hypersensitivity to Sound, Light, and Touch
During mania or hypomania, the brain feels overstimulated. Things seem too loud, lights too bright, clothes uncomfortable.
It’s not a sensory disorder, it’s your brain in overdrive. Many confuse it with anxiety or ADHD.
Rage and Sudden Irritability
Not all mania feels good. Some people get extremely irritable, aggressive, or even verbally explosive.
This is called “dysphoric mania”, and it’s one of the most commonly misinterpreted symptoms. Loved ones might assume you’re angry or abusive when really, you’re overwhelmed by internal chaos.
Hypersexuality and Risky Behavior
Increased libido and impulsivity can lead to behavior that’s out of character, risky sex, oversharing, or crossing boundaries.
This isn’t about morality; it’s a symptom of mania or hypomania. And many people feel deep shame afterward.
Obsessional Loops & Repetitive Thinking
You may play a song in your head 100 times, spiral into circular thoughts, or fixate on one idea for days.
These aren’t hallucinations; they’re intrusive thoughts fueled by elevated brain activity.
Guilt and Embarrassment After Episodes
After a manic phase, clients often tell me:
“I ruined everything. I feel disgusting.”
This crash isn’t just depression; it’s post-episode shame, and it can lead to withdrawal, substance use, or suicidal thinking.
Feeling “Emotionally Flat” Between Episodes
Some people with bipolar disorder report feeling emotionally blank or apathetic between highs and lows.
This inter-episode numbness is under-discussed but incredibly real.
How Bipolar Disorder Feels (In People’s Words)
As a psychologist, I often tell clients: “No textbook will ever describe bipolar the way you feel it.” And that’s the truth. Diagnoses help, but the lived experience? It’s raw, confusing, and incredibly personal.
Here are some real quotes from clients and community forums like Reddit and Quora that reveal what bipolar disorder actually feels like on the inside:
“When I’m manic, I feel like a genius. Like I can solve the world.”
Mania can feel empowering at first, like your thoughts are lightning-fast and everything makes sense. But this can quickly turn reckless.
“It’s like I’m vibrating on the inside, but nobody sees it.”
This invisible energy, like being wired but not focused, is often missed by others. From the outside, you might look “productive.” Internally, it’s chaos.
“I overshare with strangers. Then I avoid them for weeks.”
Hypomania can fuel social confidence and impulsivity. Later, shame and depression set in. Many people with bipolar live in this cycle of “connection → embarrassment → withdrawal.”
“I feel too much or absolutely nothing.”
Clients often say they’re either deeply sensitive crying over a song, or numb to everything. This emotional pendulum is exhausting and unpredictable.
“It’s like being drunk on thoughts.”
During manic or mixed states, people describe thoughts racing too fast to track. It’s not always grandiose, it’s disorganized. Some compare it to trying to read 20 browser tabs at once.
“I didn’t know my good moods were symptoms.”
This is a big one. Many people seek help during depression, not realizing their “good” periods were actually hypomania.
“I hate who I become in mania but I miss her when I’m depressed.”
There’s grief, too. Some clients mourn the version of themselves who felt alive, inspired, and bold, even if that version was destructive. Therapy often involves untangling that identity.
These stories remind us that bipolar disorder isn’t just a diagnosis; it’s an emotional experience. It impacts relationships, self-worth, and even memory of events.
And the hardest part? Many people are told to “calm down,” “snap out of it,” or worse are ignored altogether.
That’s why therapy isn’t just treatment. It’s validation.
Bipolar vs. BPD vs. Depression: Clearing the Confusion
Many people come to therapy unsure what they’re actually dealing with. They’ve heard terms like bipolar, BPD, and depression thrown around, and it all feels blurry. That confusion is valid because there’s a lot of overlap in how these conditions can look, especially during emotional overwhelm.
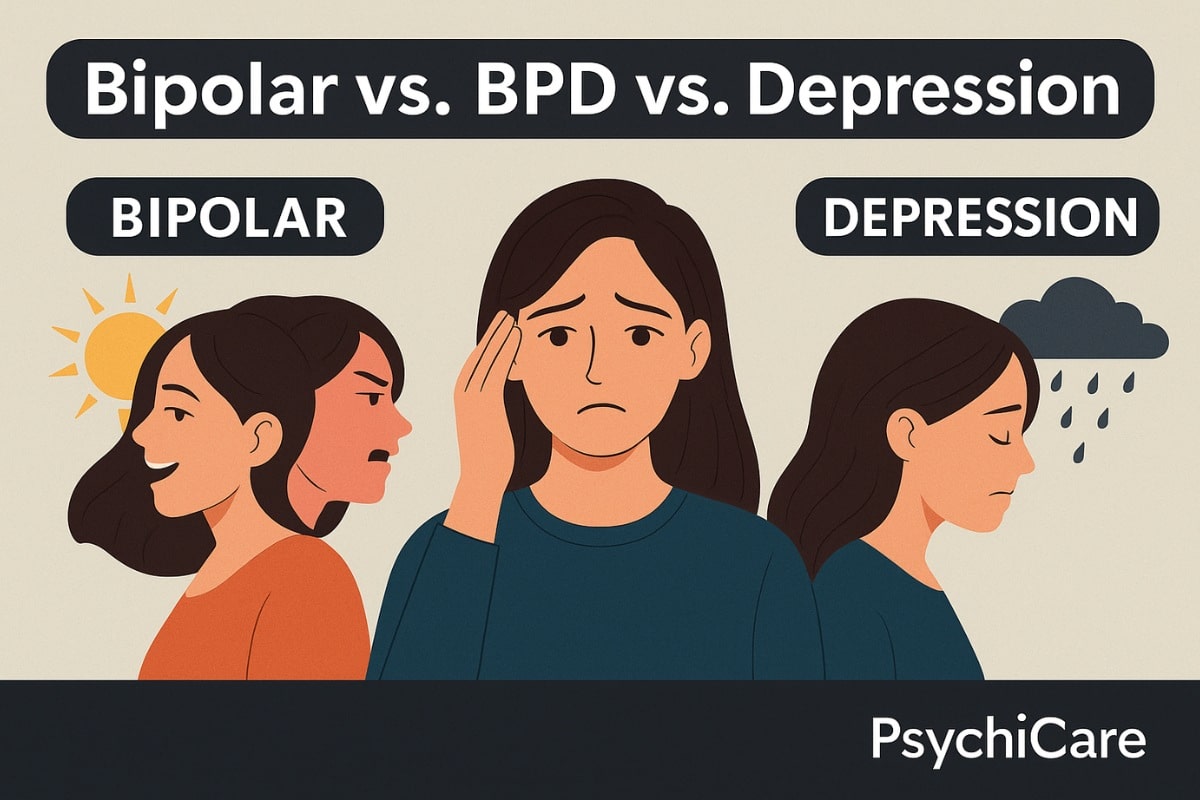
Here’s how I explain the key differences to my clients:
Bipolar Disorder
It’s a mood disorder. The emotional highs (mania or hypomania) and lows (depression) last for days to weeks. The mood shifts are often cyclical, with symptom-free periods in between.
You may feel energetic, driven, impulsive, and later, deeply low or empty. These aren’t reactions to events; they happen even when life is calm.
Borderline Personality Disorder (BPD)
This is a personality disorder. Emotions shift hour to hour, often triggered by relationships or fear of abandonment. It’s not about mania, it’s about instability in self-image, intense fears of being left, and difficulty regulating feelings.
People with BPD may struggle with self-harm, identity confusion, or extreme sensitivity to rejection.
Major Depression
Depression on its own doesn’t include manic or hypomanic episodes. It’s a long-lasting low: persistent sadness, hopelessness, and loss of interest in life.
While bipolar includes depression, not all depression is bipolar.
💡 The Big Difference
- Bipolar = mood episodes that come and go (highs & lows)
- BPD = fast emotional swings triggered by situations
- Depression = persistent low mood without highs
Triggers and Causes of Bipolar Disorder
Bipolar disorder isn’t your fault and it doesn’t mean you’re “too emotional” or “unstable.” It’s a complex condition shaped by biology, life experiences, and environment.
In therapy, I often explain it this way: your brain already has the wiring for bipolar. Certain life events and habits can flip the switch.
Let’s break it down.
1. Genetics (Family History)
If a parent or sibling has bipolar disorder, your risk increases. But it’s not a guarantee, you might inherit the sensitivity, but not the disorder itself.
This is often referred to as a genetic vulnerability.
2. Sleep Disruption
One of the most common triggers for both manic and depressive episodes is lack of sleep. Even a few nights of poor sleep can trigger hypomania in someone vulnerable.
This is why maintaining a consistent sleep schedule is often part of treatment.
3. High Stress or Trauma
Major life events like losing a job, a breakup, moving cities, or even becoming a parent, can bring out bipolar symptoms, especially if they haven’t shown up before.
Some people only notice signs after a traumatic event, which can confuse diagnosis.
4. Medication or Substance Use
Certain medications, especially steroids or antidepressants taken alone, can trigger mania. So can alcohol or stimulants like caffeine and recreational drugs.
This is sometimes called secondary mania or organic mania, and it’s more common than people realize.
5. Hormonal Changes
Puberty, pregnancy, postpartum periods, or menopause can activate symptoms in those already vulnerable.
In some clients, bipolar episodes first appeared after giving birth, and were initially misdiagnosed as postpartum depression.
6. Brain Chemistry
Research shows bipolar disorder involves imbalances in neurotransmitters like dopamine, serotonin, and norepinephrine.
These brain chemicals affect mood regulation, energy, motivation, and sleep, all of which are disrupted in bipolar episodes.
A lot of clients ask:
“Did I cause this by how I lived?”
The answer is no. You didn’t cause it, but learning your triggers can help you manage it better.
How Psychologists Diagnose Bipolar Disorder
Many people assume diagnosis means ticking off a checklist or taking a quick quiz online.
But in reality, diagnosing bipolar disorder is a process one that involves careful observation, honest conversations, and sometimes, a bit of detective work.
As a psychologist, I’ve seen how tricky this can be, especially when symptoms overlap with depression, ADHD, or trauma.
What We Look For
- Mood Episodes That Follow a Pattern
We ask about periods of:
- unusually high energy or activity
- racing thoughts or impulsive behavior
- deep sadness, low energy, or hopelessness
We’re looking at duration, intensity, and how much it affects your life, not just whether you feel happy or sad.
- How Long Have You Felt This Way?
To qualify as bipolar:
- Manic episodes must last at least 7 days (or require hospitalization).
- Hypomanic episodes last around 4 days.
- Depressive episodes typically last 2+ weeks.
Anything shorter might still be relevant, but falls into different clinical categories. - Your History, Not Just Today
A key part of diagnosis is understanding your entire mood history: - Have these episodes happened before?
- Were there clear triggers?
- Do you have family members with bipolar or other mood disorders?
We often hear, “I thought that was just a phase,” or “I’ve always been up and down.” These are clues.
- What’s Not Bipolar (But Looks Like It)
We also rule out conditions like:
- Major depression (without highs)
- ADHD (fast thoughts ≠ mania)
- Borderline Personality Disorder (rapid emotion shifts but not cyclical mood episodes)
- PTSD (emotional dysregulation from trauma)
This is why therapy takes time, there’s no blood test for bipolar. It’s a clinical diagnosis based on patterns, context, and how you’ve coped over time.
Why Many People Get Misdiagnosed
Most people seek help during a depressive episode. If hypomania hasn’t been obvious (or felt good), they may get diagnosed with “just depression.”
Later, when a manic episode appears, everything clicks into place.
That’s why I often say:
“Diagnosis isn’t a label. It’s a roadmap.”
It helps you understand why you feel the way you do and what can help.
What Therapies Help with Bipolar Disorder?
While medication plays a key role in stabilizing bipolar symptoms, therapy is where people often find understanding, structure, and long-term strategies.
In sessions, we don’t just talk about feelings; we help you spot early warning signs, manage energy shifts, and repair relationships impacted by the disorder.
Here are the most effective, research-backed therapies for bipolar disorder:
1. Cognitive Behavioral Therapy (CBT)
CBT helps you recognize thought patterns that fuel emotional spirals, like impulsive decisions during mania or hopeless beliefs during depression.
We work on:
- challenging all-or-nothing thinking
- breaking cycles of guilt and shame
- identifying “trigger thoughts” before they escalate
2. Interpersonal and Social Rhythm Therapy (IPSRT)
Bipolar disorder thrives on disruption, especially in sleep, meals, and routines. IPSRT focuses on stabilizing your daily rhythms like when you sleep, eat, and interact socially.
It helps reduce the risk of manic or depressive episodes by keeping your internal clock consistent.
3. Psychoeducation
This means learning to truly understand your diagnosis. We explore:
- The different types of bipolar disorder
- How symptoms show up in your life
- How to involve family without shame
Knowledge is power, and it helps you advocate for yourself in both medical and personal settings.
4. Family-Focused Therapy (FFT)
Bipolar disorder doesn’t just affect the individual; it impacts relationships too. FFT includes sessions with your partner or family to:
- Reduce blame
- Increase understanding
- Teach healthy boundaries and support systems
This is especially helpful when symptoms have led to conflict, confusion, or resentment in the home.
5. Mindfulness and DBT Tools
While Dialectical Behavior Therapy (DBT) is usually used for BPD, certain DBT and mindfulness strategies help bipolar clients too, especially for:
- Emotion regulation during mixed states
- Reducing impulsivity
- Staying grounded in the present
Final Thoughts From a Psychologist
If you’ve read this far, there’s likely a part of you wondering: Could this explain what I’ve been feeling? And that question alone takes courage.
Bipolar disorder isn’t just a diagnosis, it’s a lived experience that affects your energy, decisions, relationships, and how safe you feel inside your own mind.
But with the right support, you can learn to understand those cycles, spot them early, and live with greater stability and self-trust.
At PsychiCare, we’ve helped thousands of people across the world find clarity and calm in the midst of emotional chaos.
We’re proud to be recognized among the Top 10 mental health counselling platforms in India, and trusted by clients in the U.S., UK, UAE, Australia, and over 20 countries.
- ⭐ 500+ verified 5-star reviews on Google
- ⭐ 800+ therapy success stories on our website
- 🌍 Known for international online therapy and culturally sensitive care
Whether you’re newly diagnosed, misdiagnosed, or just confused by what you’re feeling, we’re here to help you figure it out.
Our therapists don’t just listen. They understand bipolar disorder from both a clinical and human perspective.
FAQs About Bipolar Disorder
1. How do I know if I have bipolar disorder or just depression?
If you’ve had periods of unusually high energy, reduced need for sleep, impulsive behavior, or feeling “on fire” with ideas even if they felt good at the time, you may have experienced hypomania or mania. That’s a key difference. A licensed psychologist or psychiatrist can help clarify your pattern.
2. Can you have bipolar disorder without being “crazy”?
Yes. Most people with bipolar disorder are not out of control or “crazy.” Many hold jobs, raise families, and live meaningful lives. The challenge isn’t being unstable, it’s often being misunderstood, untreated, or overwhelmed by internal shifts.
3. What are early signs of bipolar disorder in adults?
- Frequent mood crashes after “productive” highs
- Making big life decisions impulsively
- Irritability without reason
- Sleep disturbances (needing very little sleep, or sleeping too much)
- Feeling like two different versions of yourself over time
4. Why is bipolar often misdiagnosed?
Because people usually seek help during depression, and overlook hypomanic phases as “good days” or “confidence bursts.” Some are also misdiagnosed with BPD, ADHD, or just stress.
5. Can bipolar disorder go away on its own?
It can stabilize with age or awareness, but it rarely disappears. Without support, episodes may continue unpredictably. With treatment, people often go months or years without major symptoms.
6. Is bipolar disorder dangerous?
Untreated, it can lead to impulsive actions, financial harm, substance use, or suicidal thoughts, especially during mixed episodes. But with treatment, it’s absolutely manageable.